Leptospirosis, also known as Weil’s disease in humans, is a zoonotic disease caused by several species of spiral-shaped bacteria in the genus Leptospira. The organisms are motile and require moist environments to survive.
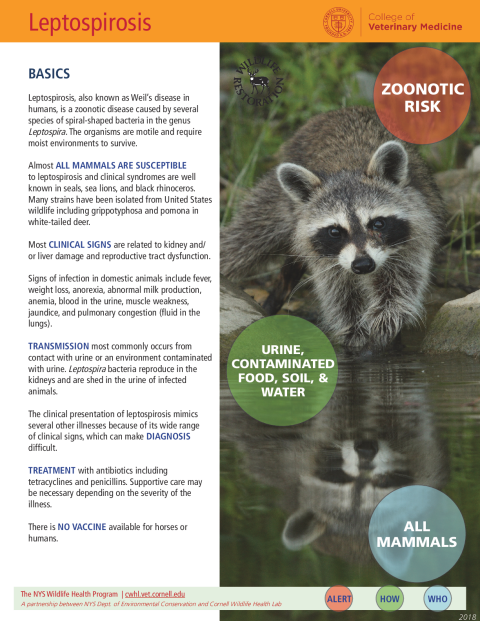
Almost all mammals are susceptible to leptospirosis and clinical syndromes are well known in seals, sea lions, and black rhinoceros. Many strains have been isolated from United States wildlife including grippotyphosa and pomona in white-tailed deer.
Most clinical signs are related to kidney and/or liver damage and reproductive tract dysfunction.
Signs of infection in domestic animals include fever, weight loss, anorexia, abnormal milk production, anemia, blood in the urine, muscle weakness, jaundice, and pulmonary congestion (fluid in the lungs).
Transmission most commonly occurs from contact with urine or an environment contaminated with urine. Leptospira bacteria reproduce in the kidneys and are shed in the urine of infected animals.
The clinical presentation of leptospirosis mimics several other illnesses because of its wide range of clinical signs, which can make diagnosis difficult.
Treatment with antibiotics, including tetracyclines and penicillins. Supportive care may be necessary depending on the severity of the illness.
There is no vaccine available for horses or humans.
Leptospires are usually organized into serologic groups called “serovars” for reference. Specific serovars of leptospires are often associated with particular animal species, or “maintenance hosts”, that are only mildly affected but able to persistently shed the bacteria.
More than 250 pathogenic serovars have been identified, many of which are specific to different regions of the world. Rats are common sources of human infections because they are the maintenance hosts for the serovars that cause disease in people.
Wild animals that are potential reservoirs include raccoons, skunks, squirrels, insectivores (moles, shrews, hedgehogs), opossums, deer, rodents, buffalo, and marsupials. Little is known about the disease in reptiles, amphibians, and fish; although antibodies to the bacteria can be found in these species, they are thought to be a minor risk for transmission to people.
The symptoms of leptospirosis vary depending on the serovar and the species. In maintenance hosts, leptospirosis may be asymptomatic. Most wildlife cases are thought to be self-limiting and asymptomatic, except for marine mammals, particularly sea lions.
In maintenance hosts that show signs, infections are mild, while illness may be more severe in incidental hosts. Incidental host infection is characterized by an acute (fast onset) systemic illness with fever.
Clinical signs in humans include fever, headache, muscle aches, vomiting, weakness, and meningitis. In more severe cases icterus (yellow pigmentation of skin) and kidney failure can occur. The overall mortality rate in humans is 1% to 5% but can vary depending on the serovar.
Human exposure can occur by swimming in water that has been contaminated by urine harboring the bacteria. Infection can also occur through sexual or social contact, across the placenta, and through ingestion of infected milk.
Leptospires can survive in infected carcasses and be transmitted to scavengers. The bacteria invade the body through the gastrointestinal tract, mucous membranes, urogenital system, upper respiratory tract, and eye. Open wounds or skin abrasions can also serve as a point of entry for the bacteria.
Diagnostic tests involve either directly identifying the organism or increasing antibodies in the blood of infected individuals. Culture is most successful during the acute stage of illness, while serologic test results must be interpreted carefully as antibodies may not be present in early illness, and prior vaccination of the animal may cause false positive results.
Leptospires can survive in the environment up to three months with favorable conditions, mainly high moisture alkaline (basic) soil or stagnant or slow-moving freshwater bodies of water. Leptospirosis outbreaks occur under favorable conditions such as following floods and monsoons. In the temperate regions, outbreaks are more common in the summer and fall. In the tropics, outbreaks are more common following the rainy seasons.
People who work with animals, including veterinarians, livestock producers, and dairy workers, are at increased risk of leptospirosis and should take appropriate preventative precautions, including wearing gloves and washing hands frequently.
Vaccines against leptospirosis are available for pigs, cattle, and dogs. Vaccination against leptospirosis should be considered for dogs at risk, but most vaccines offer only protection against the most common serovars.
Dogs may be at increased risk for leptospirosis if they hunt, swim in stagnant ponds, or live in regions with a high incidence of leptospirosis. Taking appropriate precautions can help decrease the risk of contracting leptospirosis.